More than 50 million Americans suffer from allergies each year, and allergy-related illness is the 6th leading cause of chronic illness in the U.S. The causes of allergies are as varied as the resulting symptoms. There are four types of allergic, or hypersensitivity, reactions. Check out this post to learn about Type I Hypersensitivities. Here we will delve into the mechanism and types of Type IV reactions.
Type IV Hypersensitivity Reactions Defined
Type IV reactions are delayed hypersensitivity reactions where there is no reaction to the first exposure to a substance, but subsequent exposures to the substance elicit a response. These include contact dermatitis in response to metals, poison ivy, cosmetics, or rubber gloves, as well as adverse drug reactions, multiple sclerosis, and type 1 diabetes.
Type IV delayed hypersensitivity reactions occur in two phases:
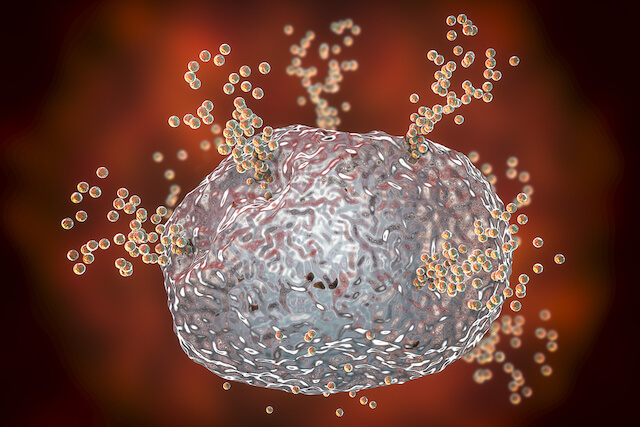
- Induction Phase: Upon the first exposure an allergen antigens react with and sensitize T-cells.
- Elicitation or Challenge Phase: Upon subsequent exposure to the same allergen, antigens contact pre-sensitized T-cells, activate macrophages, and allergic symptoms occur.
While elicitation may happen soon after induction, it may also take years for elicitation to occur.
Haptens
In plants and essential oils, antigens that participate in Type IV reactions are called haptens. From the Greek word meaning ‘to fasten’, Type IV reactions may occur when haptens enter the body through the skin and bind with peptides on specialized immune cells. The hapten-peptide complexes migrate to local lymph nodes, where they sensitize T-cells. Upon subsequent exposure, sensitized T-cells trigger an immune response in the dermis and epidermis, causing an inflammatory response.
Subcategories of Type IV Reactions
There are many different types of Type IV hypersensitivity reactions. These include contact dermatitis, pigmented contact dermatitis, irritant contact dermatitis, photoallergy, and photosensitivity.
Allergic Contact Dermatitis
Allergic contact dermatitis is the most common type of delayed hypersensitivity. It is characterized by red rash, itching, dry skin, swelling, burning, or tenderness, and in severe cases, blisters. Those at high risk for allergic contact dermatitis include health care workers, dental employees, metalworkers, house cleaners, cooks, and gardeners, as well as the chronically stressed. People with other allergies at baseline are more likely to suffer from allergic contact dermatitis.
Essential Oils and Allergic Contact Dermatitis
There is no comprehensive list of essential oils that can cause allergic contact dermatitis, nor is there great evidence to differentiate if reactions are truly allergic or merely irritant. Certain essential oils may feel hot or cold on the skin and may cause itching, redness, or irritation. Use caution with clove, lemongrass, cinnamon bark, peppermint, rosemary, oregano, thyme, basil, and cassia. If an essential oil ever causes irritation, add carrier oil.
Most skin reactions to essential oils are localized to the exposed area of skin, and skin reactions to airborne fragrances rarely occur. However, people with skin symptoms are more likely to experience eye and airway symptoms when fragrance is in the air.

The Fragrance Mix
To diagnose allergic contact dermatitis to essential oils, one study used a fragrance mix containing geraniol, cinnamaldehyde, hydroxycitronellal, cinnamyl alcohol, a-amylcinnamaldehyde, isoeugenol, eugenol, and oak moss blended in 87% petrolatum. The mixture was applied to the skin in a patch test. Approximately 11.4% of people tested experienced an allergic reaction to the fragrance mix.
The problem with this study is that most people do not apply multiple isolated chemical constituents to their skin. Instead, we open a bottle of pure essential oil and add a few drops neat or diluted to our skin or place in a diffuser. Rather than using a fragrance mix, a patch test is a better way to test for a sensitivity to specific essential oils.
Pigmented Contact Dermatitis
Pigmented contact dermatitis is similar to allergic contact dermatitis, but skin darkens instead of turning red as melanin rises to the upper dermis. People with darker skin are more likely to have this type of reaction.
Phototoxicity
Phototoxicity is very common with essential oils. Essential oils containing furanocoumarins (FCs) are the cause of phototoxicity reactions.

FCs intercalate (squeeze between) DNA base pairs. When exposed to UV light, the FCs form covalent bonds with DNA by crosslinking. This triggers an inflammatory response that causes redness of the skin, sunburn, and in severe cases, blistering. Phototoxicity symptoms may not occur for several days following exposure, and the hyperpigmentation may last for weeks.
Botanicals that can cause phototoxicity are in the Rutaceae and Apiaceae families. Most citrus essential oils cause phototoxicity. However, some citrus essential oils, like lemon leaf, satsuma, tangerine, tangelo, and yuzu, are not phototoxic.
Phototoxicity may occur in people of all skin tones. However, people with lighter skin are more susceptible, and people with albinism are at very high risk. There is no difference in risk of phototoxicity based on eye color, age, sex, or ability to suntan, though a suntan at baseline may confer some protection.
To reduce the risk of phototoxicity, do not apply essential oils high in FCs before going into the sun, and wear protective clothing and sunscreen.
Photoallergy
Photoallergy is a rare reaction where the skin reacts with UV light but does not result in a change in pigmentation. There is one reported case where sandalwood essential oil caused photoallergy, and one case with lavender essential oil. Given the rarity of photoallergy, it is not a concern to essential oil users.
Looking for more educational information about essential oils? Come